Guest blog by Margaret Jowitt
The current management of women in labour is based around RCTs of what health professionals do – or don’t do – to women under their care. Physiology comes right at the bottom of the hierarchy of evidence in evidence based medicine, but in the case of childbirth, a physiological process rather than a disease to be treated, physiology should head that list. We should be managing care according what the woman’s body needs in order to labour efficiently and effectively.
Traditionally, the forces of labour are described in terms of the Powers, the Passenger and the Passage. Somewhat bizarrely, this model denies both the mother and her baby any active involvement in the process. We can make a better model of labour when we consider the mother and her baby as active participants. The uterus is the interface between them. Both the mother and her baby have bodies which can move and affect the effectiveness of uterine activity.
It is true that in mechanistic terms the uterus is the ‘engine’ of labour. It is the strongest muscle in the body but it is acting upon that most delicate of human beings, a baby. Mistreated engines tend to seize up, sometimes with catastrophic consequences. Understanding how the uterus works is central to good maternity care but most textbooks have little to say on the subject, they simply refer to uterine function as the ‘Powers’. Contractions just happen – or not. And if not, labour can usually be kick started with artificial oxytocin.
Labour is a hormonal event. We have only to look at the effects of syntocinon (Pitocin) infusions to know that oxytocin has a very powerful effect on the uterus but physiologists are aware that blood levels of natural oxytocin do not increase until second stage. What drives labour before second stage seems to be the increasing sensitivity of the uterus to these lowish levels of oxytocin. We also know that, even in established labour, contractions can stop and that the likely mechanism is antagonism of oxytocin by the stress hormones secreted by anxious or fearful mothers. Preventing or alleviating the mother’s stress will improve uterine function. This is where supportive midwifery care comes into the picture.
But there is another driver of contraction which physiologists know about but doesn’t make the clinical textbooks and that is stretch. Most smooth muscle, including that of the uterus, is activated by stretch. That is how food moves along the intestines, faeces through the colon and blood through the veins.
The heart, a special form of smooth muscle, has a pacemaker to drive its contractions and scientists have been searching in vain for a pacemaker site in the uterus. Instead they have found that any site in the main body of the uterus has the capacity to be either a pacemaker or a pace follower. 25 years ago I proposed that fetus him/herself ‘steered’ themselves towards the exit by means of what I called the stretch-contract reflex. Visualise a balloon shaped trampoline and put a kicking baby inside. The origin of a contraction will be where the fetus is stretching the uterus. Shortly after my first book, Childbirth Unmasked, was published, Sheila Kitzinger rang me to suggest that the so-called neonatal reflexes could be involved. This was a vast improvement on my initial idea. Milani Comparetti, the father of paediatric neurology, proposed that the neonatal reflexes enabled the fetus to search for the ‘invitation to softness’. The fetus himself may kick his way into the best position for his journey through the birth canal.
Is the fetus really able to position her/himself for entry into the birth canal? Does the fetus utilise his/her reflexes to negotiate the birth canal? Could cerebral palsy be the cause of a difficult labour rather than being a consequence? We don’t know, but a role for fetal positioning in labour is a testable hypothesis. I am no lover of electronic fetal monitoring, but we would need a few expectant mothers who were willing to undergo multi-channel monitoring for a few contractions. Electromyography can already record electrical activity in the uterus at more than one place at once and the source and spread of a contraction can be mapped using powerful computer software. At the same time movement activated LED lights could be placed in a network over the mother’s abdomen and videoed to provide a corresponding map of activity. We could then see whether there was any correlation between fetal movements and uterine activity. A few contractions from a few women with babies in different positions (e.g OP, AP, breech) and with the women adopting a different position for each contraction should yield a wealth of data for a computer to crunch.
If the results supported the hypothesis, the importance of maternal freedom of movement would become apparent. The mother, her fetus and the uterus would all need to have as much freedom of movement as possible in order to enable the fetus the manoeuvre him/herself in the optimum position for birth. Restricted movement would lead to pain and failure to progress, all too often found in ‘managed’ births where electronic fetal monitoring limits mothers’ choice of position.
My most recent mindshift has been in the area of the material substance of the uterus – by which I mean the composition of the biological tissue of which it is formed. We already know that there are hormonal changes in terms of receptor sites for various contraction associated proteins (CAPs), but what if substantial changes to the gross anatomy of the uterus involving tissue remodelling was taking place during labour itself? What if the uterus started to remodel itself during labour (as we know it does during the days that follow)?
We already know that the cervix has scaffolding of collagen which keeps it shut during pregnancy and which can be artificially ripened (broken down) by prostaglandins so that it can to stretch to 10 cm in the course of labour.
The uterus also has collagen scaffolding. This is less well known – tissue samples from the main body of the pregnant uterus are harder to come by. What if uterine collagen performs the same task as the collagen scaffolding at the cervix, preventing stretch-initiated contraction? What if this collagen is also broken down (by prostaglandins, IL-8 and MMP8, collagenase) during labour? The loss of collagen scaffolding then affects the biomechanics of the uterus, allowing it to become progressively more stretchable and more contractable. The ‘trampoline’ of the uterus becomes ‘bouncier’. Contractions become more effective. The fetus starts searching for the best way out.
Now for the final piece of the puzzle, the onset of labour. We know that in other mammals the fetus is involved in initiating labour by a hormonal mechanism which changes the balance between oestrogen and progesterone, but in humans progesterone levels remain high even at the onset of labour. In order to be able to give birth to a baby with a bigger head, we evolved to give birth earlier in pregnancy when the progesterone block was still in place. Rising oestrogen does still plays a part in the onset of labour. On a signal from the fetus, oestrogen rises and primes the uterus for labour by increasing oxytocin receptors and gap junctions. The oxytocin receptors make the uterus more contractile and the gap junctions allow electrical activity to spread to involve the whole uterus.
It looks as though the alternative mechanism (from a change in the oestrogen:progesterone ratio) for the onset of human labour may be stretch-activated inflammation acting on a primed uterus. The only difference between Braxton Hicks contractions and the contractions of labour are that BH contractions are less powerful and don’t spread so far. In the oestrogen primed uterus, contractions can spread. Inflammation is a primary driver of labour, often associated with premature labour. According to Kim et al of Imperial College (unpublished paper, unknown date):
“The stimuli triggering inflammatory activation in normal human parturition are not fully understood.”
I think the elusive inflammatory event that precipitates labour is increased stretch made possible by loss of collagen, the same biochemical mechanism that causes cervical ripening. Both twin pregnancy and polyhydramnios are associated with premature labour. The uterus is already distended so it takes little more to push it over the edge into labour. Breaking the waters can kick start labour in a uterus that is already primed for labour because now the fetus is able to stretch one part of the uterus with more force.
What can we do to improve uterine efficiency?
RCTs have shown better outcomes with caseload midwifery and out-of-hospital birth. This suggests that the powerhouse of the uterus tends to work better when its owner is cared for by a midwife, preferrably a midwife already known to her. Labour progresses more quickly at home when measured by the simplest of parameters – length of labour. The Birthplace study (2011) doesn’t give average length of total labour for all women, but women giving birth in obstetric units laboured there for 9 hours and women giving birth at home had a midwife for 6.6 hours. Midwives encourage women to move freely, women are less likely to be tethered to a fetal monitor and asked to remain still. Midwives are expert in rearranging the furniture to allow women freedom of movement. Labouring in water is even better.
All women need freedom of movement, not just low risk women deemed suitable for midwife-led care. We should stop putting women to bed for labour and we should outlaw tight belts holding transducers in place, we may be preventing the very activity that we need to enhance. I found that forward leaning positions were least painful in my labours. These positions keep the main body of the uterus away from the maternal bones.
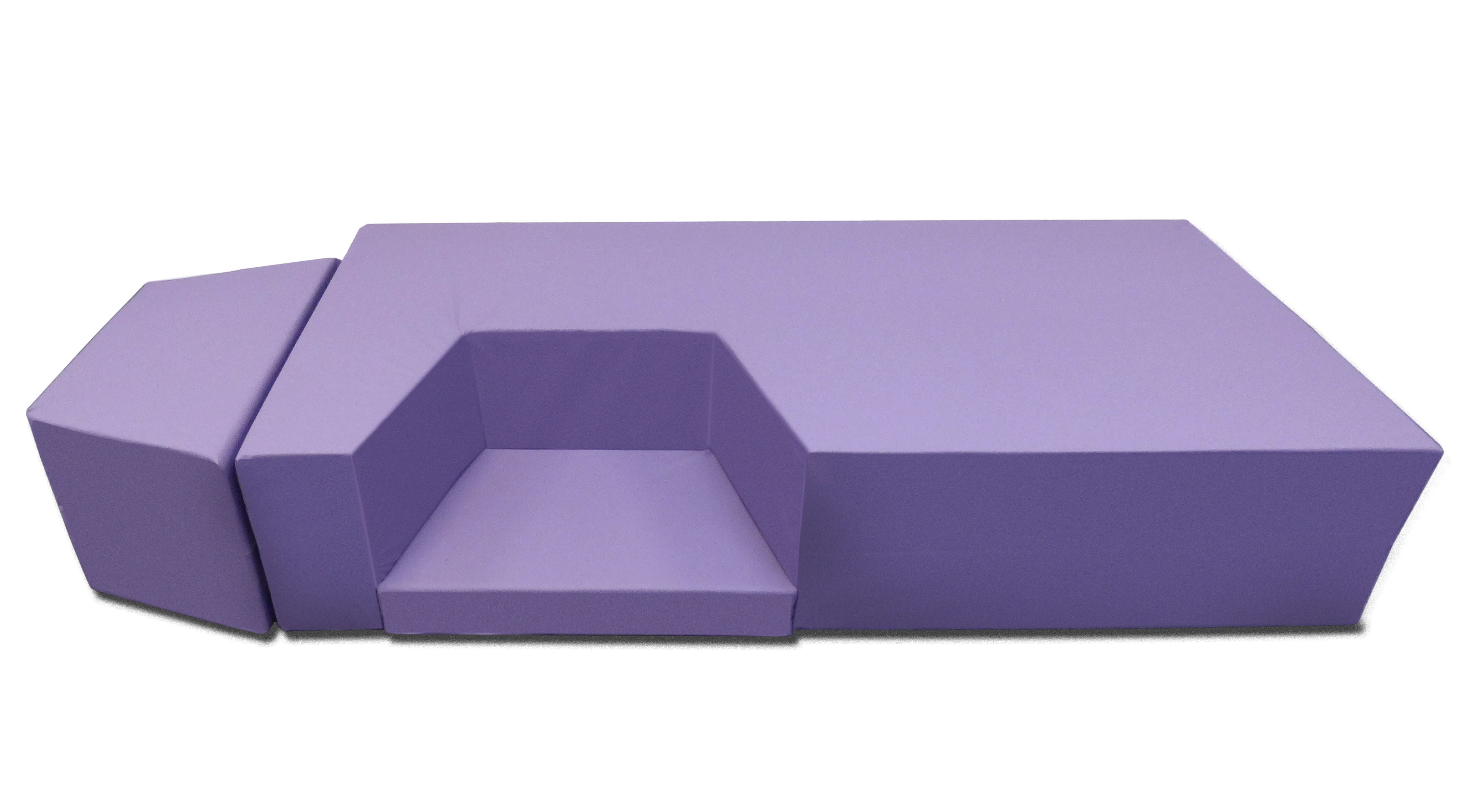
You can see a visual representation of the ‘collagen scaffolding’ on a youtube animation made to illustrate a kneeling chair I have designed for labour and birth and which, I hope, illustrates why I am so passionate about giving women freedom of movement in labour. Freedom of movement should not just be a ‘nice to have’ option for low risk women but a physiological imperative for all women in labour. (In case you were wondering, freedom of movement should also include freedom to choose the bed!)